Tympanoplasty
Tympanic surgery for simple perforations is known as myringoplasty (or, more rarely, type I tympanoplasty). As soon as the surgery requires more, it is referred to as a tympanoplasty, since associated procedures on the ossicles, mastoid and auditory canal can be added if necessary. So there are several types of tympanoplasty to suit every problem. The operation is performed under general anaesthetic by an ENT surgeon, and requires hospitalization for 1 or 2 days.
Find out more about tympanoplasty from Dr. Delagranda, ENT and cervico-facial surgeon
and cervico-facial surgeon in La Roche sur Yon
Indications and objectives of tympanoplasty
Tympanoplasty is indicated in cases of :
- Repeated infections (otitis).
- Tympanic retraction.
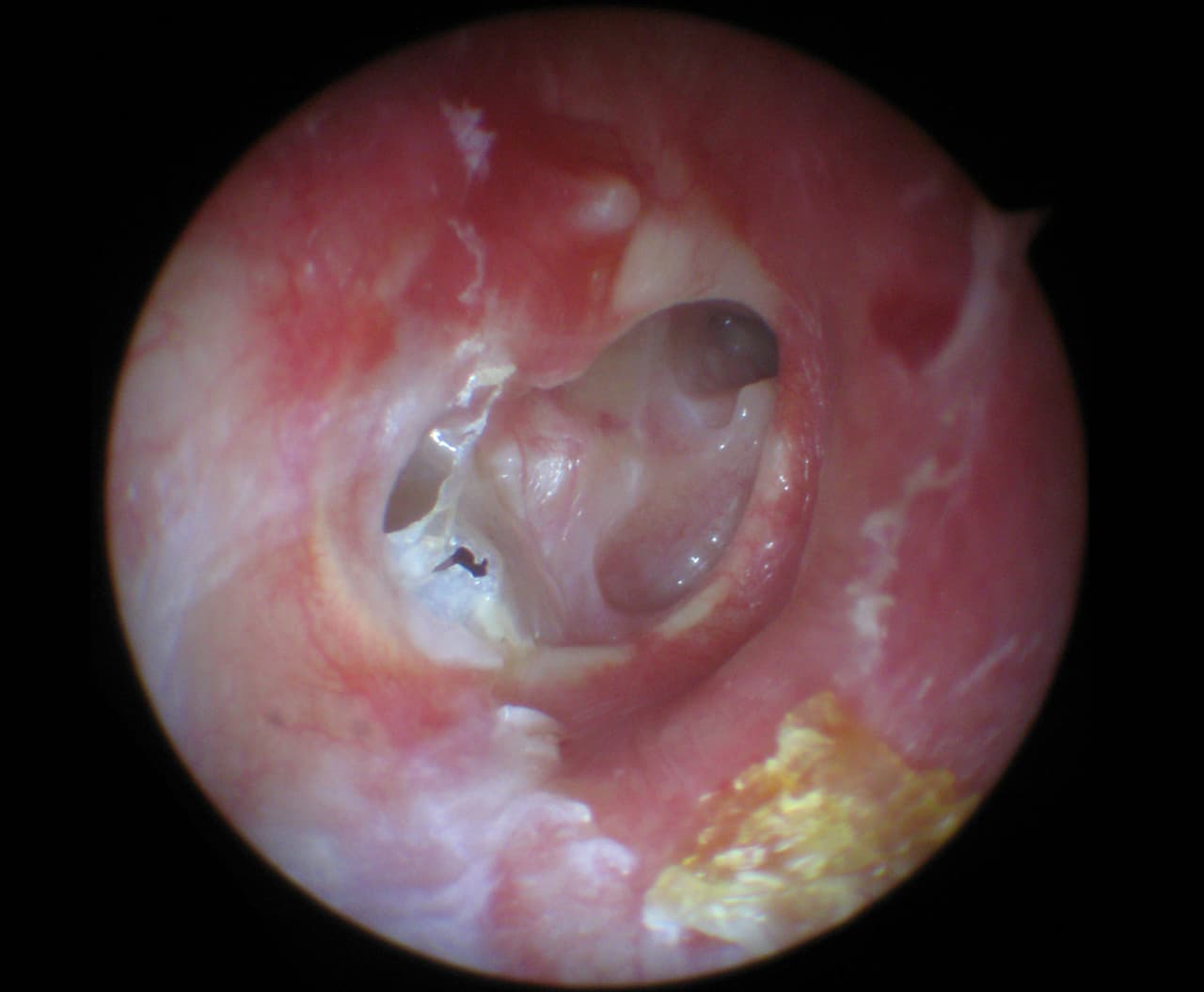
- Cholesteatoma: acquired in 98% of cases, most often from a retraction pocket in the upper part of the tympanum (pars flaccida towards the attic), congenital in 2%.
- Destruction by chronic infection or fracture of the ossicles: rupture of ossicular continuity and consequent reduction in sound transmission.
Objectives of tympanoplasty are:
- Improve hearing (ossicle replacement or plasty, prosthesis fitting).
- Prevent serious complications of cholesteatomas: meningitis, facial paralysis, vertigo, total loss of hearing (cophosis), brain abscess.
- Stop permanent discharge (chronic otorrhea).
Eardrum and middle ear
The eardrum is a membrane that separates the outer ear from the middle ear and forms the end of the external auditory canal. It is shaped like a flattened cone, like a Chinese hat, with the tip pointing towards the inside of the skull. The tip, which corresponds to the point of attachment of an ossicle: the malleus, is only 2 mm deeper than the edges. Its average height is 10 mm and its width 8 mm. It is slightly downward and outward-facing in its most anterior part, so its surface area is larger than the cross-section of the external auditory canal, i.e. around 60 mm2. It has 2 distinct zones separated by integrated tympanomalleolar ligaments. The S-shaped external auditory canal partially protects it from external mechanical stress:
The pars tensa: located below the ligaments, this accounts for the greater part of the eardrum (85%). This portion is the most rigid. From outside to inside, it is made up of three layers: an epithelial layer, which is the continuity of the skin of the auditory canal and outer ear; a fibrous layer, the lamina propria, containing collagen fibers; and a mucous layer, which is the innermost layer. The eardrum’s plasticity and elasticity enable it to vibrate in response to sound.
The pars flaccida or schrapnell membrane, above the ligaments, is smaller (15%) but lacks the intermediate fibrous layer that makes it more fragile.
The middle ear or tympanic cavity is an air-filled cavity between a cylinder and a cube, bounded by the eardrum on the outside and bone on the other sides. It contains the three ossicles, which are free to move because of the air surrounding them: the hammer (7-9mm), the anvil (5-7mm) and the stirrup (2-4mm). Three nerves pass through the middle ear: the ˝chorda tympani˝ of the tympanic membrane, which is involved in the sense of taste, the facial nerve, which controls motor activity in the hemi-face, and the Jacobson’s nerve, which innervates the mucous membrane of the middle ear. The middle ear communicates with the rhinopharynx via the eustachian tube, with the mastoid via the aditus ad antrum, and with the inner ear via the oval and round windows.
The middle ear and eardrum can be the site of multiple pathologies within different nosological frameworks: congenital malformation (e.g. ossicular agenesis or aplasia), chronic infections (e.g. chronic otitis destroying ossicles or stiffening the eardrum), tympanic retraction, flaccid eardrum, presence of destructive skin in the middle ear (cholesteatoma).
Who is concerned by tympanoplasty?
- Adults or children with hearing loss related to ossicular and/or eardrum pathology.
- Adults or children with progressive tympanic retraction or tympanic retraction that cannot be controlled in consultation.
- Adults or children with cholesteatoma (possible permanent foul-smelling discharge from the ear, reduced hearing).
- Adults with repeated otitis externa due to water blockage in the auditory canal by exostoses (bone growth reacting to cold water): Bathers, regular surfers.
Bear in mind that your ENT surgeon may suggest a tympanoplasty when you yourself have few or no clinical signs. Tympanoplasty can be a preventive measure to avoid complications of your pathology, which until now have been of little concern. A retraction can turn into a cholesteatoma, which in turn can lead to serious complications such as meningitis, facial paralysis, vertigo, total loss of hearing (cophosis) or cerebral abscess.
The different stages of the intervention
The surgical procedure
The procedure is performed under general anesthesia in the operating room, either as an outpatient or after a 2-day hospital stay. A tiny skin incision of 1 to 1.5 cm is made, either in front of the ear, extending above and behind, or a little further back (3-4 cm), depending on the technique chosen by the surgeon. The procedure varies according to the cause (removal of the cholesteatoma, mastoid milling, reconstruction of the bony framework, tympanic reconstruction and stiffening, replacement of ossicles with a titanium prosthesis, or recutting of bridged ossicles). A healing dressing is placed in the ear canal for 10 to 15 days.
Post-surgery recovery period
If you are hospitalized as an outpatient, you can go home the same day, or the following day.
After hospitalization, you must remain at home for 10 days, resting and not putting any liquid in your ear other than the prescribed drops.
The surgeon will give you 10 to 15 days off work.
Sport is not recommended for the first 15 days, and should be resumed gradually.
Swimming and diving are not recommended until your surgeon has advised you.
Flying is not recommended for 2 months.
Pain is slight, sometimes increased when chewing. It is soothed by class I analgesics such as paracetamol, and usually disappears within a week.
Post-operative care at home: ear drops to keep the healing dressing moist and effective, ear protection, analgesics, nursing care of the scar.
Scar: The scar depends on whether or not the mastoid needs to be reamed. It may be in the auditory canal, just in front of the ear (1-1.5 cm), hidden behind the hairline, or longer, extending above and behind the ear (canal route, endaural, extended endaural): it all depends on the procedure to be performed. It is barely visible in the long term, as it is very lateral on the face.
Complications associated with tympanoplasty
In addition to the risks inherent in any surgery involving general anaesthesia, tympanoplasty presents risks of complications or failure:
- Like any graft, it may fail to book and necrose, leading to failure to close the perforation.
- Appearance of mild, temporary taste disorders, such as the erroneous perception of a metallic taste.
- Narrowing of the auditory canal due to retractive scarring.
- No or minimal hearing gain.
- Hearing reduction or loss
Exceptional complications are linked to the extent of inflammatory lesions and bone destruction in the ear:
- Dizziness
- Meningitis
- Facial paralysis
For further information, please consult the ENT College’s explanatory sheet on tympanoplasty:
➔ Exostose du conduit auditif externe
➔ Intervention pour otite moyenne chronique chez l’enfant et l’adulte
Frequently asked questions about tympanoplasty
Here is a selection of questions frequently asked by Dr Delagranda’s patients during consultations for tympanoplasty in La Roche-sur-Yon.
When should I have an operation on my eardrum and middle ear?
Contact your ENT surgeon, who will be able to advise you. Even with few symptoms, an operation is sometimes necessary.
Fees and coverage for the procedure
Tympanoplasty is covered by the French health insurance system. Contact your mutual insurance company to find out how much coverage there is for any extra fees.
Do you have a question? Need more information?
Dr Antoine Delagranda will be happy to answer any questions you may have about tympanoplasty. Dr Delagranda is a specialist in ENT surgery at the Clinique Saint Charles in La Roche-sur-Yon in the Vendée.
ENT consultation for tympanoplasty in Vendée
Dr Antoine Delagranda will be happy to answer any questions you may have about tympanoplasty. Dr Delagranda is a specialist in ENT surgery at the Clinique St-Charles, La Roche sur Yon, France.

