Turbinoplasty
Turbinoplasty is a surgical procedure on the lower turbinates, always performed by an ENT surgeon, but which may vary from one practitioner to another. In all cases, the aim is to improve nasal permeability. Some surgeons remove part of the lower turbinates, while others induce sclerosis of the mucosa, either by contact heat or radiofrequency in the turbinates. For reasons of medical conviction, I do not perform turbinectomy, which consists in removing part of the bone of the lower turbinates, in order to avoid empty-nose syndrome.
Who is concerned and when a turbinoplasty should be performed?
Turbinoplasty concerns adults with a blocked, runny nose, especially if it’s unilateral and tilts from one side to the other.
Children over 15, for the same reasons.
Turbinoplasty should be performed in cases of :
- Sensation of a blocked nose, especially if it is unilateral and tilts from one side to the other.
- Runny nose, especially if unilateral and tilting from one side to the other.

Lower turbinates
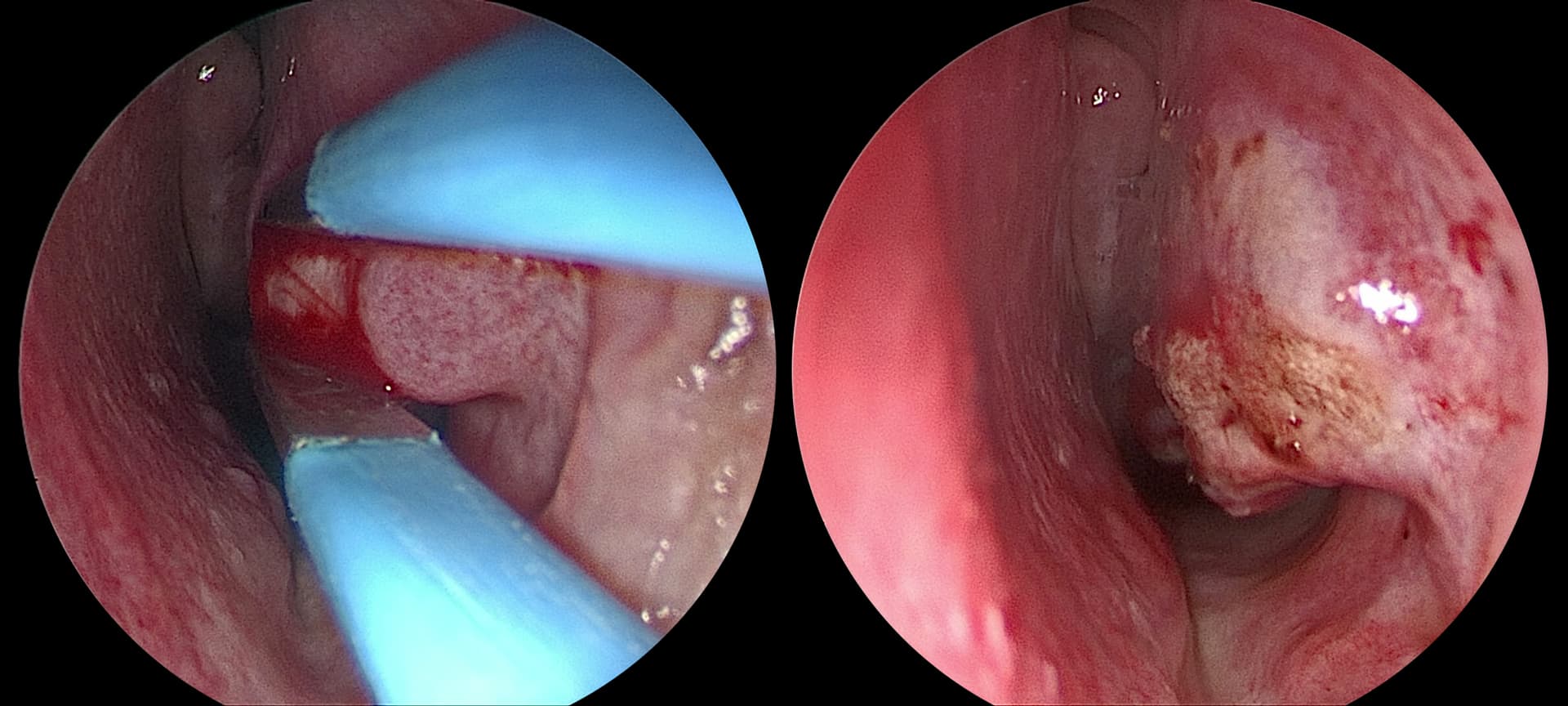
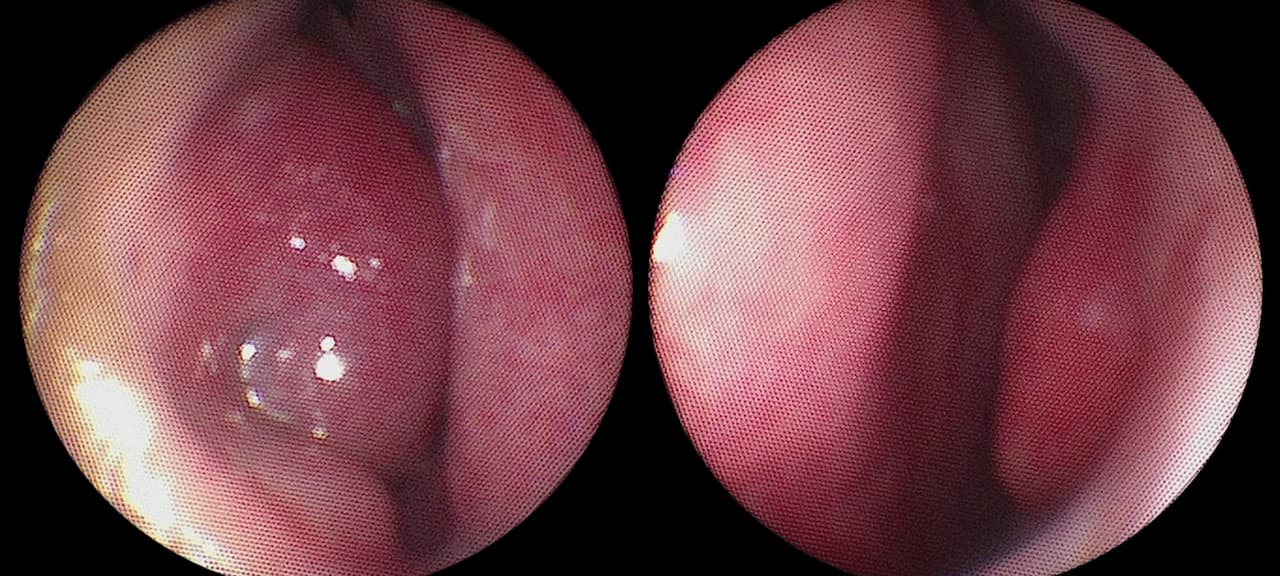
The turbinates are small bones in the lower, lateral part of the nasal cavity, covered by a special mucous membrane with an erectile capacity that regulates the heat and humidity of inspired air, optimizing gas exchange in the lungs. This mechanism of increasing or decreasing mucosal thickness and mucus secretion in response to external climatic conditions is cyclical and alternates between the right and left sides: it’s known as the nasal cycle. Present in the majority of people without discomfort, in some it is exacerbated and a source of discomfort. Allergic problems should be considered before any action is taken on the turbinates.
Objectives of turbinoplasty
- Achieve a sensation of freer airflow through the nasal cavity on inspiration.
- Reduce anterior or posterior rhinorrhea (runny nose) and thus sniffling or chronic coughing.
- Encourage the use of CPAP (continuous positive airway pressure).
- Optimize the work of the orthodontist.
The different stages of the intervention
The surgical procedure
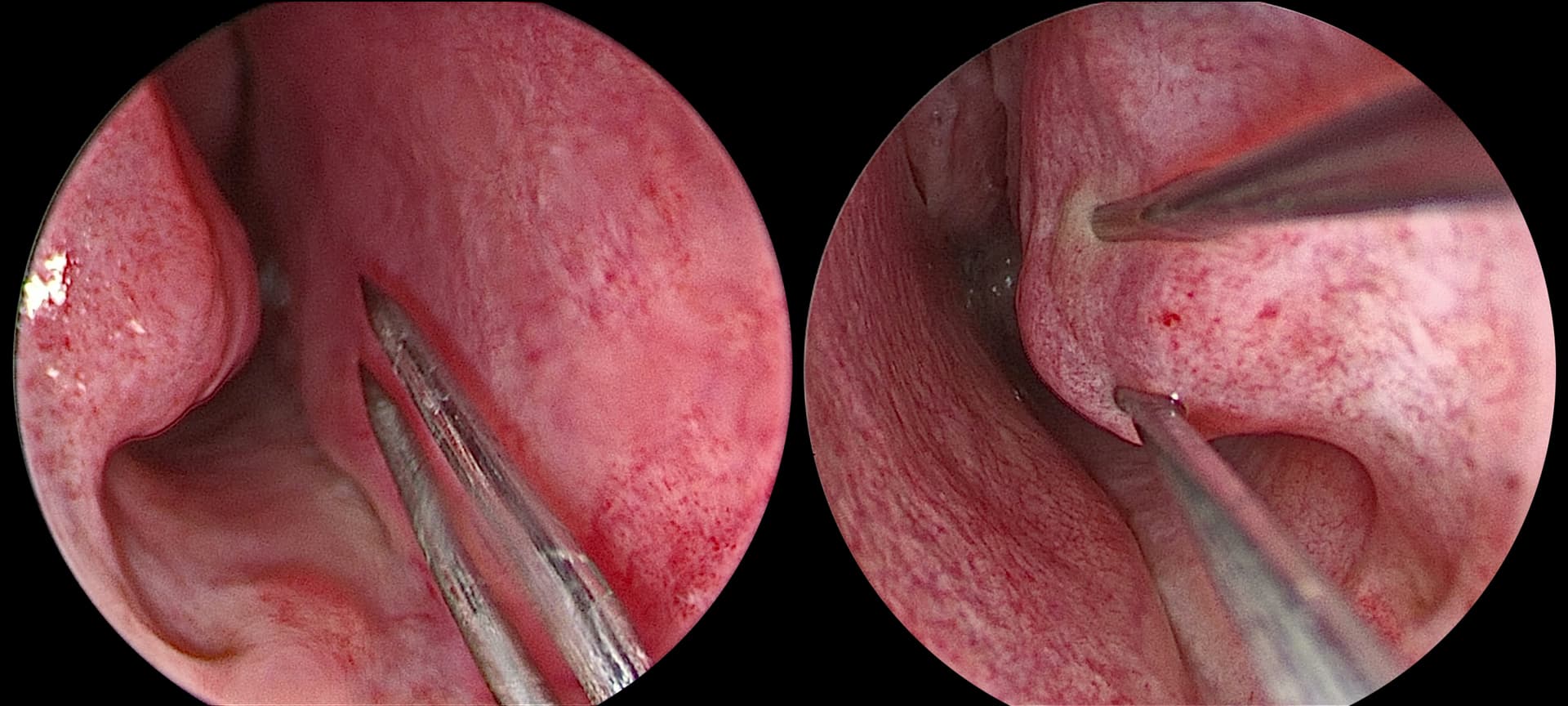
Under local anaesthetic in the operating theatre or in the consultation room, depending on the conditions, and more rarely under general anaesthetic, the procedure consists of either applying a calibrated electric current directly to the mucosa (thermal action), or pricking the lower turbinates and applying a radiofrequency for 20 seconds between the 2 ends of an electrode, following a topical and/or injected local anaesthetic under visual control with an optic introduced into the nose. No wick or product is placed in the nose after the procedure, which lasts around fifteen minutes, including anesthesia time.
Post-surgery recovery period
Return home is immediate.
No time off work. Pain is minimal and short-lived. Class I analgesics are used to control pain.
Post-operative care at home: nose washed with saline several times a day for 21-30 days until all crusting has disappeared.
Scarring : no visible scar.
Precautions: none
Complications associated with turbinoplasty
Apart from the risks inherent in any surgery with local anesthesia, turbinoplasty does not present any risk of complications except for :
- Very moderate, small-volume nasal bleeding (a few minutes).
- Scar adhesions in the nose that can restrict airflow. This can be corrected secondarily.
- Surgical site infection.
- Bad odor perceived in the nose as long as there are endonasal crusts.
- Watery eyes.
- The effect of turbinoplasty varies from person to person, and can be either permanent or temporary (6 months). The procedure can be repeated if necessary, with sufficient time between procedures.
Please consult the ENT College’s explanatory sheet on turbinoplasty for further explanations and exceptional complications:
Frequently asked questions about turbinoplasty
Here is a selection of questions frequently asked by Dr Delagranda’s patients during turbinoplasty consultations in La Roche-sur-Yon in the Vendée.
Is the operation compulsory?
No, it is purely functional.
Is the result immediate?
No, you may have to wait several weeks before you feel the full benefits, especially if you have nasal crusts. Frequently, there is an improvement in the first 15 days, then a decline in benefits over the following 15 days with the appearance of nasal crusts before the expected nasal permeability is fully felt.
Does turbinoplasty alter the functions of my nose?
No. The intensity of the bipolar coagulation or radiofrequency electrode is adjusted in such a way as to have no detrimental effect.
Fees and coverage for the procedure
Turbinoplasty is covered by the French health insurance system. Contact your mutual insurance company to find out how much coverage there is for any extra fees.
Do you have a question? Need more information?
Dr Antoine Delagranda will be happy to answer any questions you may have about turbinoplasty. Dr Delagranda is a specialist in ENT surgery at the Clinique Saint Charles in La Roche-sur-Yon in the Vendée.
ENT consultation for turbinoplasty in Vendée
Dr Antoine Delagranda will be happy to answer any questions you may have about turbinoplasty. Dr Delagranda is a specialist in ENT surgery at the Clinique Saint Charles in La Roche-sur-Yon in the Vendée.