Stylohyoid syndrome or Eagle syndrome
Stylohyoid syndrome is commonly referred to as Eagle syndrome, after the American surgeon who studied and popularized it in 1937, although Weinlecher was the first to perform endobuccal surgery in 19th-century Europe, and Loeser and Caldwell the firsts to perform cervical surgery in 1942.
The operation consists of removing the distal part of the styloid process and the stylohyoid ligament, if ossified.
Find out more about the treatment of the eagle syndrome from Dr. Delagranda, ENT and cervico-facial surgeon in La Roche sur Yon (France).
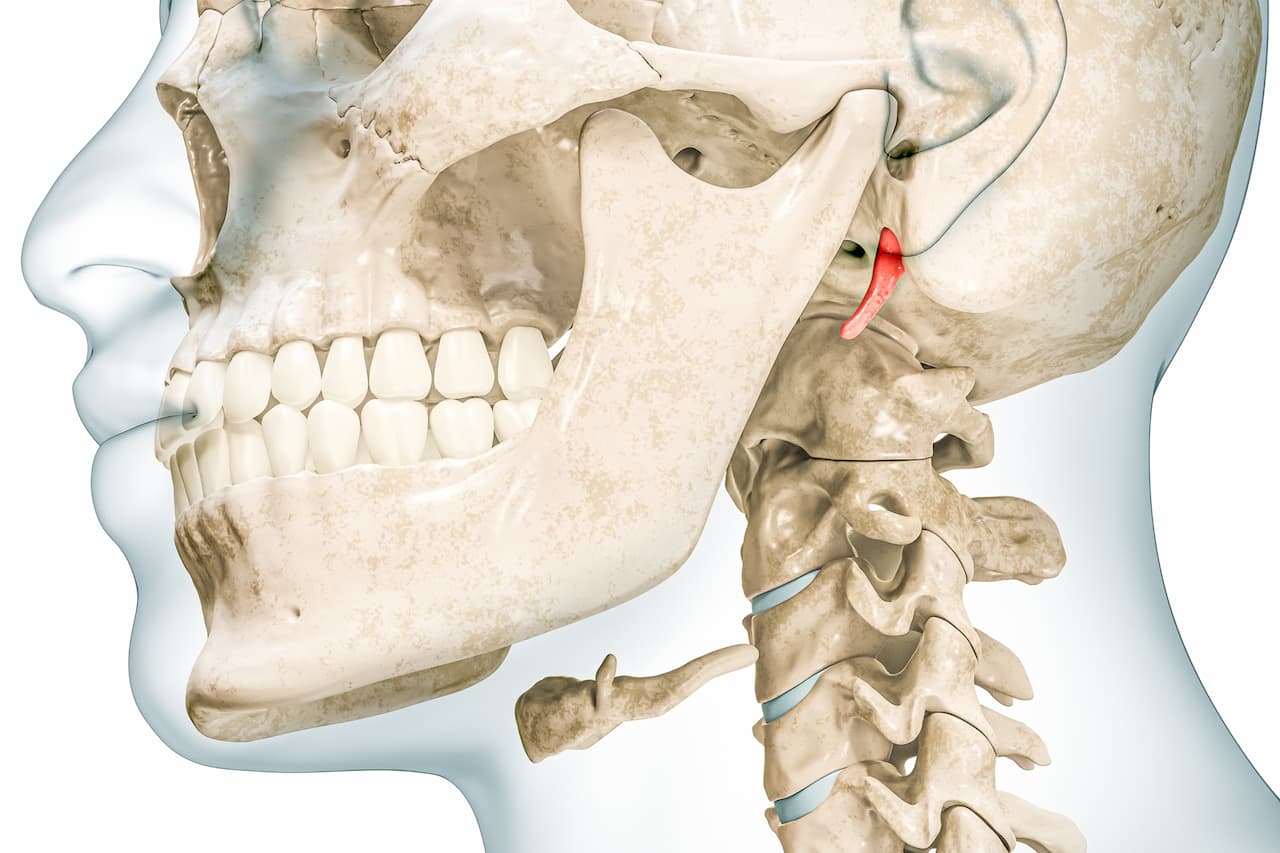
Styloid process and Eagle syndrome
The styloid process or styloid apophysis is a part of the temporal bone located on its lower part in its petrous zone, forming a point directed downwards, forwards and inwards, with major variations in size and angulation between individuals, and sometimes even between the 2 sides of the same individual. There is a styloid process under the skull on each side, as there are 2 temporal bones. The styloid process is often less than 3 cm long, with a starting diameter of 4 mm and a terminal diameter of 1 mm. Its base of implantation is next to the mastoid styloid foramen, from which the facial nerve emerges, some of whose lower branches may be quite close in this surgery. Its tip is the site of implantation of 2 ligaments (stylohyoid and stylomandibular) and 3 muscles (styloglossal , stylohyoid , stylopharyngeal). The tip may be in contact with the internal carotid artery, external carotid artery, and nerves (adventitial sympathetic plexuses, sensory branches of cranial nerves V , VII, IX, X). Other valuable anatomical elements are to consider in this surgery including the XII nerve and lingual artery, which may also be in close proximity.
A styloid process length greater than 3 cm would certainly increase the risk of Eagle’s syndrome, however 15.4% of cases with Eagle’s syndrome would have a styloid process of less than 3 cm according to Cheng C (Am journal Otolaryngology head and neck surgery 2017) and in 34.5% of cases of totally healthy patients, the styloid process would be greater than 3.5 cm according to Buyuk C (Folia morphol 2018; 77 :79-89). So the presence of a long styloid is not a sufficient criteria to speak of Eagle syndrome.The active ossification of embryonic cartilaginous remnants of the tip of the styloid process and of the stylohyoid ligament, and even of stylial muscles in adulthood, can be attributed to various etiopathogenic hypotheses: genetic predisposition, menopause, osteoporosis, osteoarthritis, repeated straining by carrying heavy cephalic loads, very late effects of tonsillectomy, direct trauma, etc.
Diagnosis of Eagle syndrome
The diagnosis of Eagle syndrome is rare, and relatively difficult because it is unknown by many doctors, and made up of variable and aspecific functional signs. As a result, many sufferers allege aches and pains, sometimes for years on end, before a diagnosis is made. Clinical examination and palpation, on the other hand, are very helpful in diagnosis, as is cervical CT imaging. Thus, a styloid process can be considered pathological if it is palpable and painful in the tonsil compartment. The fact that this palpation triggers a pain identical to the one usually perceived spontaneously by the patient is a strong argument, especially if it is unilateral. A CT scan showing mostly asymmetric ligament calcifications and thickening of the carotid bulb wall is a further argument for diagnosis. Compression is radiologically visible in 50% of cases, with severe neurological symptoms. Carotid dissection is even possible.
There are numerous differential diagnoses: dental problems, temporomandibular joint problems, cervical infections, cervical tumors, spinal pathologies, Arnold’s occipital nerve neuralgia, glossopharyngeal nerve neuralgia, upper laryngeal nerve neuralgia, trigeminal nerve neuralgia, nasal nerve neuralgia (Charlin’s syndrome), tendinitis of the stylomandibular ligament at the level of the hyoid bone (Albert’s syndrome), hyoid bone bursitis, vascular pain, migraine, gastroesophageal reflux etc… A psychological or psychiatric cause remains a diagnosis of elimination.
The symptoms of stylohyoid syndrome are detailed below.
Who is concerned by removal of the distal portion of the styloid process?
Adults with symptoms associated with stylohyoid syndrome, whose diagnosis is based on a cluster of arguments and not on a single symptom.
- Adults with intense, stabbing, permanent or iterative, pharyngeal and/or cervical and/or auricular and/or ocular and/or mandibular and/or cranial and/or spontaneous facial pain with no other obvious causes to suggest.
- Adults with pain triggered by swallowing, cervical rotation and yawning, identical to the above.
- Adults with pain triggered by endopharyngeal palpation of the styloid tip in the tonsillar compartment, identical to the pain they usually perceive spontaneously.
- Adults with pharyngeal foreign-body sensations, globus.
- Adults with swallowing difficulties (dysphagia), taste disorders, trismus.
- Adults with balance problems, tinnitus.
- Adults with speech difficulties (dysphonia).
In 12.5% of cases, the discovery of stylohyoid syndrome follows more serious events:
- Adults with a genuine stroke of carotid origin whose side is compatible (motor deficits, visual disturbances, language disorders) by compression of the stylohyoid complex on the wall of an internal or common carotid artery. The stylopharyngeal muscle may be involved if triggered by ipsilateral cervical rotation.
- Adults with unlabelled malaise, dizziness, drop attacks, epileptic seizures.
Children are not affected by this pathology, which often appears with delayed ossification.
When should the distal portion of the styloid process be removed?
The distal portion of the styloid process should be removed if stylohyoid syndrome is suspected:
- Intense, throbbing or iterative pharyngeal and/or cervical and/or auricular and/or ocular and/or mandibular and/or cranial and/or spontaneous facial pain with no other obvious cause.
- Pain of the same localization as above, triggered by swallowing, cervical rotation or yawning.
- Pain of the same localization as above, reproduced by endopharyngeal palpation of the styloid tip in the tonsillar region.
- Sensations of pharyngeal foreign body, globus.
- Difficulty swallowing (dysphagia), taste disorders, trismus.
- Balance disorders, tinnitus.
- Difficulty speaking (dysphonia).
- Severe neurological disorders associated with styloid tip and carotid artery compression-dissection (stroke).
- Unlabelled malaise, dizziness, drop attacks, epileptic seizures.
Objectives of the removal of the distal portion of the styloid process are:
- Alleviate pain.
- Reduce pain.
- Prevent recurrence of carotid stroke.
The different stages of the intervention
The surgical procedure
Medical treatment (analgesics, non-steroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, injections of NSAIDs or anesthetics into the tonsil cavity) should be reserved for patients with a formal surgical contraindication. In fact, medical treatment does not induce a cure, only momentary relief.
Endobuccal surgery, even if it gives satisfactory results (73.9%), is not to be recommended as it does not control all the risks, whereas cervical surgery offers better results (84.2%) and better control of vessels and nerves (Lisan Q, Management of stylohyoid syndrom: a systematic review following prisma guidelines, European annals of otorhinolaryngology, head and neck diseases 136 (2019) 281-287).
Under general anesthesia, with tracheal intubation, without prolonged curarization, in the operating theater, the skin of the neck is incised 4 to 6 cm below and behind the mandibular angle, in a natural fold if possible. Muscles (sterno cleido mastoid and mylo hyoid), carotid arteries, lingual artery and nerves (XII and sometimes VII) are identified and preserved. Then approach and palpate the styloid tip and the stylohyoid ligament, in order to cut them and remove a 2-3 cm length And finally, if necessary, blunt the remaining styloid process to avoid residual pain. Closure is performed either directly or with drainage, depending on dissection (decision taken intraoperatively).
Surgical treatment does not rule out failure, as diagnosis of certainty is impossible and differential diagnoses are numerous.
Post-operative recovery period
The patient is usually discharged home the following day, or the day after in the case of weekday hospitalization for aspiration drainage.
After hospitalization, you should rest at home for at least 7 days.
If necessary, the surgeon will give you 7 to 15 days off work.
Sport is not recommended for the first 15 days, and resumption should be gradual.
Pain is moderate. It is controlled by class I or II analgesics.
Post-operative care at home: daily nursing care of the external scar.
Scar: cervical, arciform, 4 to 6 cm behind the mandibular angle.
Complications associated with the removal of the distal portion of the styloid process?
In addition to the risks inherent in any surgery involving general anaesthesia, removal of the distal portion of the styloid process carries the risk of rare or exceptional complications:
- Fibrous scarring, compromising the result.
- Delayed healing.
- Hematoma.
- Infection.
- Subcutaneous emphysema.
- Temporary facial paralysis in the lower part (lower lip and neck) in 1.2% of cases.
- Impaired mobility of hemi-tongue.
- Residual pain.
- Depressive syndrome.
There is no specific explanatory sheet from the College of ENT on surgery for stylohyoid syndrome, but a similar one on cervical curage can be consulted: Medical information prior to lymph node dissection (French)
Frequently asked questions about stylohyoid syndrome
Here is a selection of questions frequently asked by Dr Delagranda’s patients during consultations for removal of the distal portion of the styloid process in La Roche-sur-Yon.
Is the operation mandatory?
No, the surgeon advises and the patient decides.
Is the effect long-lasting?
Yes, but an exceptional partial regrowth of the styloid process due to the presence of cartilaginous remnants is possible, without however prejudging a reappearance of symptoms. (Steinman EP. A new light on the pathogenesis of the styloid syndrome. Arch Otolaryng 1970 ;91 :171-174).
Is it painful?
Moderately.
Fees and coverage
Removal of the distal portion of the styloid process is covered by health insurance. Contact your mutual insurance company to find out whether any extra fees will be covered.
Do you have a question? Need more information?
Dr Antoine Delagranda will be happy to answer any questions you may have about the removal of the distal portion of the styloid process. Dr Delagranda is a specialist in ENT surgery at the Clinique Saint Charles in La Roche-sur-Yon, Vendée.
ENT consultation for removal of the distal portion of the styloid process in Vendée
Dr Antoine Delagranda will be happy to answer any questions you may have about stylohyoid syndrome. Dr Delagranda is a specialist in ENT surgery at the Clinique Saint Charles in La Roche-sur-Yon in the Vendée.

